Abstract
Background: Complement dysregulation has been documented in the molecular pathophysiology of COVID-19 and recently implicated in the relevant pediatric patient inflammatory responses.
Aims: Based on our previous data in adults, we hypothesized that signatures of complement genetic variants would also be detectable in pediatric patients exhibiting COVID-19 signs and symptoms.
Methods: We prospectively studied consecutive pediatric patients from our COVID-19 Units (November 2020-March 2021). COVID-19 was confirmed by reverse-transcriptase polymerase chain reaction (RT-PCR). Patient data were recorded by treating physicians that followed patients up to discharge. DNA was obtained from peripheral blood samples. Probes were designed using the Design studio (Illumina). Amplicons cover exons of complement-associated genes (C3, C5, CFB, CFD, CFH, CFHR1, CFI, CD46, CD55, MBL2, MASP1, MASP2, COLEC11, FCN1, FCN3 as well as ADAMTS13 and ΤHBD) spanning 15 bases into introns. We used 10ng of initial DNA material. Libraries were quantified using Qubit and sequenced on a MiniSeq System in a 2x150 bp run. Analysis was performed using the TruSeq Amplicon application (BaseSpace). Alignment was based on the banded Smith-Waterman algorithm in the targeted regions (specified in a manifest file). We performed variant calling with the Illumina-developed Somatic Variant Caller in germline mode and variant allele frequency higher than 20%. Both Ensembl and Refseq were used for annotation of the output files. A preliminary analysis (A) for the identification of variants of clinical significance was based on annotated ClinVar data, while a further and more selective analysis (B) was performed to identify missense complement coding variants that may biochemically contribute to the deregulation of innate responses during infection. This analysis was mainly based on the dbSNP and UniProt databases and available literature.
Results: We studied 80 children and adolescents, 8 of whom developed inflammatory syndromes (MIS-C group). Among them, 41 were hospitalized and eventually all survived.
In our preliminary analysis, patients exhibited heterogeneous variant profiles including pathogenic, benign, likely benign, and variants of unknown significance (median number of variants: 97, range: 61-103). We found a variant of ADAMTS13 (rs2301612, missense) in 39 patients. We also detected two missense risk factor variants, previously detected in complement-related diseases: rs2230199 in C3 (33 patients); and rs800292 in CFH (36 patients). Among them, 40 patients had a combination of these characterized variants. This combination was significantly associated with the presence of dyspnea (p=0.031) and cough (p=0.042). Furthermore, 27 patients had a pathogenic variant in MBL2 (rs1800450), and 7 a pathogenic deletion in FCN3 that have been previously associated with inflammatory syndromes.
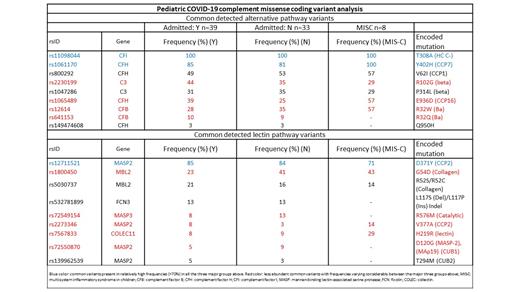
The results of our further analysis are summarized in Figure. We identified common variants, some well represented by relatively high frequencies (>70%) (rs11098044 in CFI, rs1061170 in CFH and rs12711521 in MASP2) and others less abundant, but varying considerably between the hospitalized group, the non-admitted group and the MIS-C individuals (rs2230199 in C3, rs1065489 in CFH, rs12614 and rs641153 in CFB, rs1800450 in MBL2, rs2273346 and rs72550870 in MASP2, rs72549154 in MASP3 and rs7567833 in COLEC11, all highlighted in Figure in red).). Structurally, the majority of these common variants of interest encode charge reversal mutations. These may influence protein-protein interactions in complex formations that are important for complement activation and/or regulation.
Conclusion: In pediatric COVID-19 we have detected a novel set of complement missense coding variants some of which have been implicated earlier in inflammatory syndromes and endothelial stress responses. Certain combinations of mutations of alternative and/or lectin pathway components may increase the threshold dynamics of complement consumption and therefore alter COVID-19 phenotypes.
Gavriilaki: Alexion, Omeros, Sanofi Corporation: Consultancy; Gilead Corporation: Honoraria; Pfizer Corporation: Research Funding. Anagnostopoulos: Abbvie: Other: clinical trials; Sanofi: Other: clinical trials ; Ocopeptides: Other: clinical trials ; GSK: Other: clinical trials; Incyte: Other: clinical trials ; Takeda: Other: clinical trials ; Amgen: Other: clinical trials ; Janssen: Other: clinical trials; novartis: Other: clinical trials; Celgene: Other: clinical trials; Roche: Other: clinical trials; Astellas: Other: clinical trials .

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal